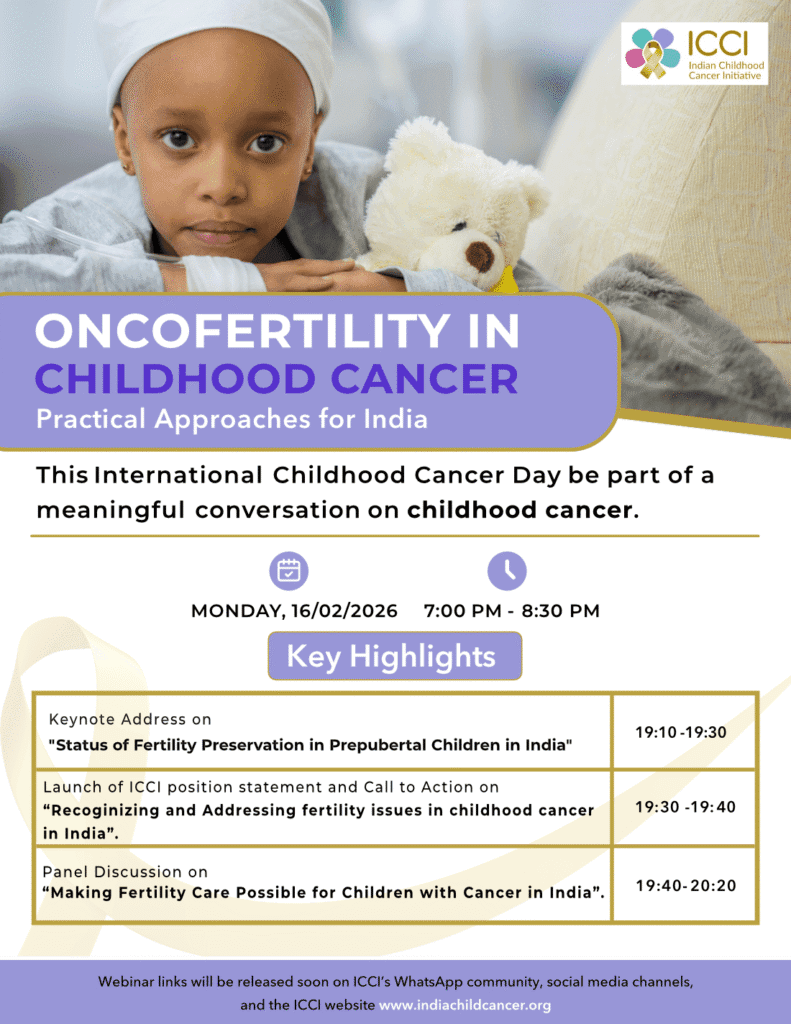
Beyond the Cure: Preserving Fertility and Future Hope for Childhood Cancer Survivors in India
International Childhood Cancer Day (February 15) is not just about the fight for survival; it is about ensuring that the life saved is lived to its fullest potential. As medical advancements increase survival rates, the focus of care is shifting from simply “curing the cancer” to “preserving the quality of life” for survivors.
At CIFAR IVF Centre, under the guidance of Dr. Puneet Rana Arora, we believe that every child fighting cancer deserves the hope of a future family. Oncofertility—the bridge between oncology and reproductive medicine—is the frontier where this hope is preserved.
Here is a perspective on the status of oncofertility in India and how we are addressing it at CIFAR.
1. Status of Fertility Preservation in Prepubertal Children in India
The most vulnerable group in oncofertility is prepubertal children. Unlike adults or adolescents, these children do not produce mature eggs or sperm, meaning standard freezing methods (like egg or sperm banking) are not options.
In India, this area has historically been a significant gap in care. However, the narrative is changing. Dr. Puneet Rana Arora, a pioneer in this field and a founder member of the Fertility Preservation Society of India, has been instrumental in bringing advanced experimental and established techniques to India.
- What are The Challenges we are facing: Prepubertal gonadal tissue (ovarian or testicular) is highly sensitive to chemotherapy and radiation.
- The Status: While still niche, Ovarian Tissue Cryopreservation is now a viable reality for young girls. For young boys, Testicular Tissue Freezing ((Experimental) is available, though it remains largely experimental globally. CIFAR IVF Centre is one of the few centres in North India actively championing these advanced options to ensure that age is not a barrier to future parenthood.
2. Recognizing and Addressing Fertility Issues in Childhood Cancer in India
The primary hurdle in India is not the lack of technology, but the lack of timely conversation and awareness. Often, the urgency to start cancer treatment overshadows the discussion about long-term side effects like infertility.
- Recognizing the Risk Factor: Chemotherapy and radiation can deplete the “ovarian reserve” in girls and damage sperm production in boys, leading to premature menopause or permanent azoospermia.
- Addressing the Gap: Addressing this requires a “Multidisciplinary Handshake.” Oncologists and fertility specialists must work in tandem. Dr. Puneet Rana Arora advocates for a “Fertility Consult before Chemo” protocol. Even a short window of 24–48 hours is often enough to counsel parents and harvest tissue or gametes without delaying cancer treatment.
3. Making Fertility Care Possible for Children with Cancer in India
Cost and accessibility are often cited as barriers. CIFAR IVF Centre is dedicated to democratizing this care.
- Collaboration: Through partnerships with NGOs like Cankids-Kidscan & Indian Cancer Society, Dr. Arora works to ensure that financial constraints do not stop a family from preserving their child’s fertility.
- Awareness: Making care possible starts with education. Parents need to know that infertility is a likely side effect of treatment, but it is also a preventable one.
Dr. Puneet Rana Arora’s Advice & Patient-Centric Approach
As the Founder & Director of CIFAR IVF Centre, Dr. Puneet Rana Arora advocates a philosophy of “Empathy backed by Science.”
Her Advice to Parents and Oncologists:
- “Preserve before you Treat”: Fertility preservation should be considered a “medical emergency” in the timeline of cancer care. It should be discussed at the time of diagnosis, not after recovery.
- Transparent Counseling: Parents are often overwhelmed. Dr. Arora emphasizes counseling that is ethical and realistic. Parents must understand what is standard care (like sperm banking for teens) versus what is experimental (like tissue freezing for toddlers), so they can make informed decisions.
- Holistic Support: Her patient-centric approach acknowledges that this is an emotional trauma. The CIFAR team provides not just medical intervention, but psychological support to help families navigate these difficult choices. Visit : https://www.cifarivf.com/cifar-support-groups/
Medical Treatments Offered by CIFAR IVF Centre
CIFAR IVF Centre is equipped with state-of-the-art technology to offer a comprehensive Oncofertility Programme tailored to the patient’s age and diagnosis.
For Post-Pubertal Children (Adolescents & Teens):
- Sperm Cryopreservation (Sperm Banking): The standard gold care for adolescent boys. It is non-invasive and effective.
- Oocyte (Egg) Freezing: For adolescent girls who have started menstruating.
- Embryo Freezing: An option for older, married patients.
For Prepubertal Children (Before Puberty):
- Ovarian Tissue Cryopreservation: A laparoscopic procedure where a part of the ovary is removed and frozen. It can be transplanted back into the patient years later to restore fertility and hormonal function.
- Testicular Tissue Cryopreservation (Experimental) : Removing and freezing testicular tissue containing stem cells for young boys (currently the only option for this age group).
Protective Measures (Adjuncts):
- Ovarian Transposition: Surgically moving the ovaries away from the field of radiation to protect them from damage.
- GnRH Agonists: Medical suppression of the ovaries during chemotherapy to potentially reduce toxicity (used alongside other methods).
Let us promise our children not just a life after cancer, but a future full of possibilities.

Add Your Comment